Therapeutic Plasma Exchange
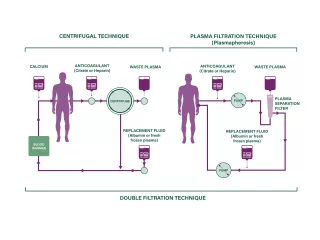
An extracorporeal blood purification technique designed for the removal of large molecular weight substances.1
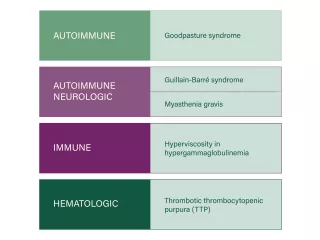
Guillain-Barré syndrome
Several controlled trials indicate that TPE can accelerate motor recovery, decrease time on the ventilator and speed of attainment of other clinical milestones compared with supportive care alone.2
Thrombotic thrombocytopenic purpura
TPE has decreased overall mortality of immune-mediated TTP from nearly uniformly fatal to <10-20%.2
Myasthenia gravis
TPE in myasthenia gravis works rapidly. Clinical effect can be apparent within 24 hours of treatment; however, in some cases it may take a week. Concomitant immunosuppression must be initiated or modified for sustained control of myasthenia gravis activity.2
Anti-glomerular basement membrane disease (Goodpasture syndrome)
A randomized controlled trial involving a small number of patients showed that TPE maintained kidney function and improved survival.2
ASFA guidelines
The American Society for Apheresis (ASFA) publishes comprehensive guidelines for therapeutic apheresis. The ASFA evidence-based approach assigns diseases to categories based on a stringent review of the literature, analysis of quality of evidence and strength of recommendation derived from the evidence.
Important Safety Information
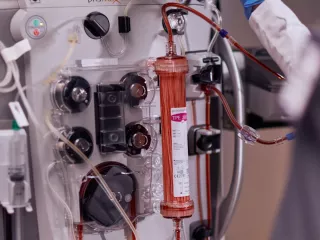
The PrisMax control unit is intended for:
- Continuous Renal Replacement Therapy (CRRT) for patients weighing 20 kg or more with acute renal failure and/or fluid overload.
- Therapeutic Plasma Exchange (TPE) therapy for patients weighing 20 kg or more with diseases where removal of plasma components is indicated.
All treatments administered via the PrisMax control unit must be prescribed by a physician.
Rx Only. For safe and proper use of the products mentioned herein, please refer to the appropriate Operator’s Manual or Instructions for Use.
Vantive and PrisMax are trademarks of Vantive Health LLC or its affiliates.
References
-
Kaplan AA. Therapeutic plasma exchange: core curriculum 2008. Am J Kidney Dis. 2008;52(6):1180-1196.
-
Padmanabhan A, Connelly-Smith L, Aqui N, et al. Guidelines on the use of therapeutic apheresis in clinical practice — evidence-based approach from the Writing Committee of the American Society for Apheresis: the eighth special issue. J Clin Apher. 2019;34(3):171-354.
-
Schwartz J, Padmanabhan A, Aqui N, et al. Guidelines on the use of therapeutic apheresis in clinical practice-evidence-based approach from the Writing Committee of the American Society for Apheresis: The Seventh Special Issue. J Clin Apher. 2016;31(3):149-162.